Ankylosing Spondylitis Print Page
Overview
Ankylosing Spondylitis is an autoimmune disease which causes back pain and stiffness. It most commonly occurs in young men, but men and women of any age can have Ankylosing Spondylitis. While there is no cure, treatment options for Ankylosing Spondylitis have improved over the last few years with good therapeutic options available.
Frequently Asked Questions
What is Ankylosing Spondylitis?
- Most people with Ankylosing Spondylitis, or AS, complain of lower back pain and stiffness, caused by inflammation. However, AS can affect any part of the spine, including the neck, upper and middle back.
How common is Ankylosing Spondylitis?
- AS is not a common disease, with less than 1% of the population having a diagnosis. It is more common in men than women, with the first manifestations often occuring as a young adult.
Could I have prevented AS? Why does Ankylosing Spondylitis happen?
- Because we do not fully understand why AS happens, there is nothing we know that could prevent it.
- The exact cause of AS remains unknown. It is possible an unidentified trigger initiates the immunologic process which causes inflammation.
- A number of different genetic markers have now been identified which increase the risk of developing AS, although no one marker completely explains the cause.
I heard something called HLA B27 causes Ankylosing Spondylitis?
- HLA B27 is a genetic marker found in approximately 8% of the general population.
- While most people with HLA B27 DO NOT have AS, most people with AS are B27 positive.
What are the common symptoms of Ankylosing Spondylitis?
- Ankylosing Spondylitis causes “inflammatory back pain”. Unlike regular back pain which affects the lower back and is best first thing in the morning and worse with activity, inflammatory back pain is associated with back stiffness in the morning, often lasting at least 1 hour, and improves with activity. It most often involves the lower back, but can affect the entire spine.
How is Ankylosing Spondylitis diagnosed?
- Your physician will listen closely to your history of back pain and for any other clues that may suggest you have AS. If diagnosed early, there may be no findings on clinical exam, although many patients have difficulty moving their back through a full range of motion.
Are there any tests to confirm Ankylosing Spondylitis?
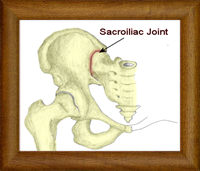
- The most common test is an X-ray of the sacroiliac joints in the hip, as this area is most often involved. However, if caught very early, there may be no X-rays changes yet. If your doctor still suspects AS, they may arrange an MRI of your sacroiliac joints, as an MRI can detect early signs of inflammation before they are seen on a X-ray.
- Your physician may order certain blood tests to look for inflammation and rule out other diagnostic possibilities, but none of these are specific.
- Because HLA B27 is so common in the general population, it cannot diagnose AS. Therefore, it is not necessary for most patients.
Besides my back, can AS affect any other joints?
- AS can also involve other large joints including the shoulders, hips, and knees. Chest involvement is also described. A minority of patients will have smaller joints affected too.
Does AS only affect joints?
- The attachment between tendons or ligaments to bone can also become inflamed and cause pain. Common examples include the Achilles tendon in the ankle, the plantar fascia on the bottom of the heal, and the patellar tendon at the knee.
- There are a number of other diseases which are commonly associated with Ankylosing Spondylitis and may give your physician a clue that your back pain is from an inflammatory cause. Common examples include inflammation of the eye, called uveitis, psoriasis, and Crohn’s Disease or Ulcerative Colitis.
- Other organ involvement can also occur, although less common, including heart, lungs, and kidneys.
Is there a cure for Ankylosing Spondylitis?
- There is still no cure for AS, but treatment options are improving, with a majority of patients having good results and able to live their lives normally.
How is AS treated?
- There are two important first steps in the treatment of Ankylosing Spondylitis. They are:
- Physiotherapy – Daily exercise and stretching regimes maintain and improve back mobility, and help maintain correct back posture.
- Anti-inflammatories (NSAIDs) – NSAIDs reduce pain and swelling, and improve day to day function. There is some evidence it may slow down the disease process, but this remains unclear.
What happens if NSAIDs do not work for me, or if I cannot take them?
- There are a number of different options available in this situation. For most patients, a TNF Antagonist would be the next preferred treatment choice. For other patients, an X-ray guided glucocorticoid injection or bisphophonates (a medication used in osteoporosis) may be options. Analgesic medication may play a role for some patients too.
For more information on ankylosing spondylitis, please discuss it further with your physician.