Osteoarthritis Frequently Asked Questions Print Page
What is Osteoarthritis?
- Osteoarthritis, or OA, is a degenerative disease of the joints. It usually occurs because of excessive loads across otherwise normal joints. Genetics can also play a role, particularly with osteoarthritis of the hand.
What other names are there for OA?
- OA has also been referred to as Degenerative Joint Disease. In the spine, it is sometimes referred to as Degenerative Disc Disease.
How common is osteoarthritis?
- OA is the most common joint disorder. It increases with age; In patients over the age of 65, 10% have knee OA and 5% hip OA which causes them difficulties.
- OA is more common in women than men.
Are there any other risks for developing OA?
- Obesity, joint damage from old injuries and smoking are some of the more common risk factors associated with OA.
What are the typical symptoms of OA?
- Patients with OA describe pain in the involved joints. It is better with rest and worse with activity, but remains painful at rest in some patients. There is sometimes a cracking or grinding sound heard when moving the joint. You may notice bony enlargement of the joints with decreased range of motion. This is often seen as nodes on the finger joints. Some patients feel stiff in the affected joints in the morning, but usually for less than one hour.
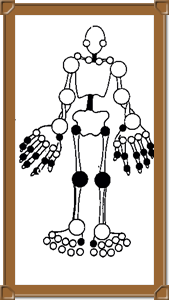
Joints that may be affected typically by Osteoarthritis are marked in black.
Which joints are affected by OA?
- Typical joints include the hips, knees, the distal joints in the fingers, and the base of the thumbs and toes.
Is Osteoarthritis the same thing as Rheumatoid Arthritis?
- No, while both cause joint problems, they are actually very different diseases. The cause, pattern of joint involvement and joint pain require different treatment approaches. Please go to the page on rheumatoid arthritis for more information.
How is Osteoarthritis diagnosed?
- OA is a clinical diagnosis made by your physician based on your medical history and an appropriate physical examination.
Isn’t there a blood test or x-ray to confirm the diagnosis?
- Blood tests do not help in the diagnosis of osteoarthritis. While an x-ray can be helpful, not everyone who has the symptoms of OA has typical changes on their x-rays. Conversely, there are many people who have x-rays changes which are consistent with OA but do not have any symptoms.
Is there a cure for OA?
- Unfortunately, we do not have a cure to reverse the degenerative effects of osteoarthritis. Treatment is based on alleviating the symptoms of OA. For best results, patients can combine different treatment modalities to work together.
I don’t like taking medications. Is there anything I can do to help my OA?
- There are many non-pharmacologic to help in the management of OA. Please discuss these options with your physician for further information. They include:
- Weight loss
- Joint brace
- Joint splinting
- Walking aids e.g. cane, walker
- Exercise to maintain strong muscle around affected joints
- Heat or cold therapy
- Water therapy and exercise including swimming & aquasize
- A relatively new program to Alberta and Canada is called GLA:D, emphasizing education and exercise to improve osteoarthritis.
Are there any medications recommended for OA pain?
- There a number of different options available, usually starting with over-the-counter acetaminophen. Others include anti-inflammatories such as ibuprofen (Motrin or Advil), and naprosyn (Naproxen or Aleve), as well as stronger prescription pain medications. You should all discuss these options with your physician to ensure their safe and appropriate use for you.
What about joint injections?
- A joint injection is a good option for some patients with OA, particular when only one or two joints are affected, such as the knees. A joint injection, either with cortisone or viscosupplementation, can be done a few times a year, and if effective, may decrease your need for regular pain medication.
What is the long term prognosis for osteoarthritis?
- While OA never goes away, it is difficult to predict if it will continue to get worse and if so, how quickly. Reducing risk factors. regular exercise, maintaining a healthy weight, and smoking cessation may all be helpful. If pain ever becomes so poorly controlled that medications are not effective, or OA is limiting your activity too much, it may be time to consider joint replacement therapy.
More Information: